COVID-19 is taking its toll on mental health worldwide. The ongoing health and economic crises are causing enormous loss, change and uncertainty and disrupting support networks and essential services. Symptoms of stress, anxiety and depression spiked during the initial months of coronavirus outbreaks and lockdowns (see Exhibit 1); two-thirds of companies that offer employee assistance programs (third-party counseling services) saw their use increase. The outlook is grim, as there is typically a lag between major events and increased demand for support, and some drivers, such as distributed working, will outlast the pandemic. An echo pandemic of mental ill health is on its way.
Even before the pandemic, mental ill health cost U.S. employers $80–$100 billion and the U.K. economy 70 billion pounds annually ($94 billion) in health care expenses and productivity losses. Against a backdrop of growing need, stretched budgets and chronic clinician shortages, it’s no wonder that employers and insurers are looking for affordable solutions at scale — two-fifths of global health insurers are considering adding video-chat counseling services to group benefits plans. As new diagnoses increase and pre-existing illnesses worsen, employees increasingly need and expect such support to sustain their well-being and productivity.
The Promise of Digital Tools: Complementing Traditional Services
A recent report from Marsh McLennan explores how digital tools can help employers support more people across key phases of mental ill health: prevention, detection, treatment, and recovery or management. Apps such as Calm and Headspace provide information and self-help guidance to raise awareness, reduce some risk factors and teach healthy coping skills such as meditation or mindfulness. Platforms such as Ginger, SilverCloud, Unmind and Togetherall connect users virtually to mental health professionals for counseling and treatment or to peers for support and social connections. Innovative detection tools are exploring the possibilities for monitoring digital biomarkers or phenotypes passively to discern signs of risk or relapse, intervene early and tailor treatments.
Digital tools can help lower long-standing barriers to access and use of mental health services — such as stigma, lack of awareness, waiting times, inconvenience and cost. Digital tools offer anytime, anywhere anonymous access — they can educate vast numbers of workers, reduce stigma and isolation, and empower them to seek timely and appropriate support. Other potential gains include reduced waiting times, increased frequency of interventions and improved outcomes: Patients who receive computerized cognitive behavioral therapy while waiting for in-person or teletherapy sessions do better than patients who wait without digital support.
Also, digital tools can reduce per capita costs, either by combining traditional and digital interventions in ways that reduce overall clinician time, or by scaling up services — for example, online resilience training can reach more people than in-person training for the same cost. For employers and insurers, digital tools can help identify unnoticed areas of need by collecting aggregate data on stress hotspots, service gaps and utilization barriers. For example, quizzes in a frequently used app can chart users’ well-being, adding to an employer’s own surveys that are often hobbled by low completion rates or insurers’ incomplete claims data.
The Pitfalls: Limitations and Risks
Digital tools for mental health are not a cure-all, and employers and insurers need to offset and mitigate key limitations, risks and concerns — including fragmented offerings, uncertain effectiveness, privacy and data security, and the exclusion of vulnerable groups.
Digital tools are typically point solutions to specific problems for certain population groups, lacking continuity over time or with physical health. The sheer number of digital tools makes selection difficult and their costs can add up. Many tools lack conclusive evidence of effectiveness in real-world conditions, and quality standards are non-existent, as in the U.S., or not mandatory, as in the U.K. In addition, digital tools vary in the extent to which they protect users’ data privacy and security, provide clinical safety nets or vet therapists’ qualifications.
Mental health equity is another challenge. With mental health services excluded from employee health benefits in many countries, digital tools and traditional services are often out-of-pocket expenses. This makes support unaffordable for many workers who need them the most — such as women, low-income workers and minorities, who experience a greater burden of mental ill health and are disproportionately affected by the health and economic crises. As for physical ill health, forgoing or deferring necessary interventions worsens conditions, delays recovery and raises costs.
Realizing Digital Tools’ Potential
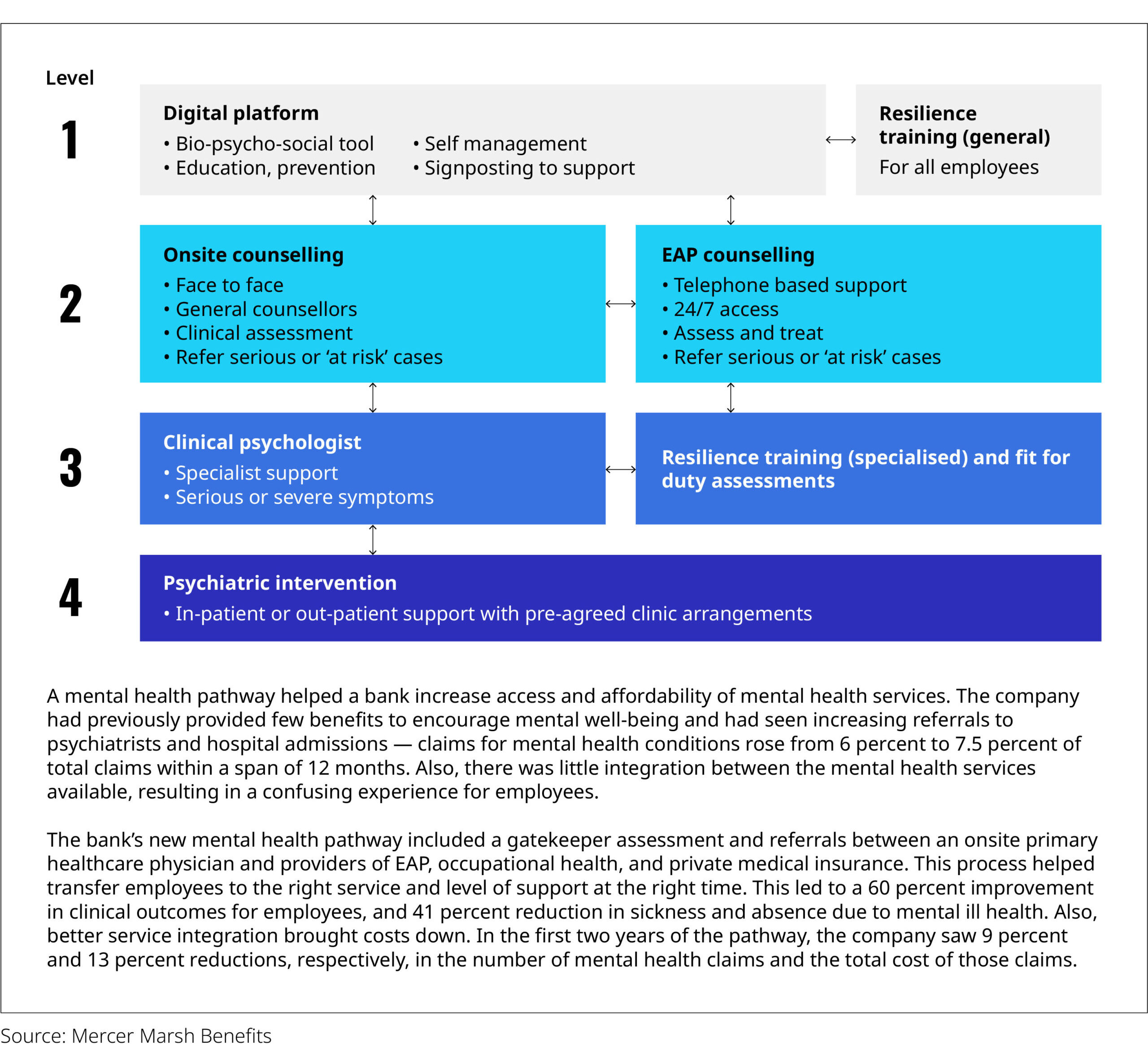
To deploy digital tools effectively, employers (or insurers) will need to collaborate with solution providers to curate a suite of evidence-based, engaging and secure tools and services that meet the mental health needs of their workers or members — and then guide employees toward the right services at the right time, such as through a mental health pathway.
Exhibit 2: A Holistic Mental Health Pathway
Communication, coverage and safeguards will be crucial to facilitating take-up. Timely, tailored and repeated communication about available tools and services are vital to make employees aware of them. Employers and insurers will need to cover the selected tools and services to ensure everyone can afford them. Equally vital is creating trust through transparency on data arrangements, precautions and safeguards against misuse or abuse of sensitive data, and emphasis on anonymity and confidentiality.
Even the best digital tools are not enough to secure workers’ mental health, so a further imperative is to create healthier workplaces and societies. Two in three employees globally felt at risk of burnout even before the pandemic. In every crisis there is an opportunity; COVID-19 presents businesses with a chance to identify and alleviate workplace risk factors — such as low pay, low job control or unmanageable workloads — and more broadly to support and protect the well-being of employees who endure chronically stressful environments and experiences. Equally important is a culture of openness and psychological safety around mental health, which requires a change set from the top.
Digital tools have the potential to play a part in empowering workers, employers and insurers with information and support to secure mental health — if stakeholders offset their limitations and create inclusive cultures that prioritize well-being. Employers that get this right will foster enduring employee trust and engagement, enjoy productivity gains and lower health care costs.